The Maxwell Finland Award for Scientific Achievement honors scientists who have made outstanding contributions to the understanding of infectious diseases and public health.
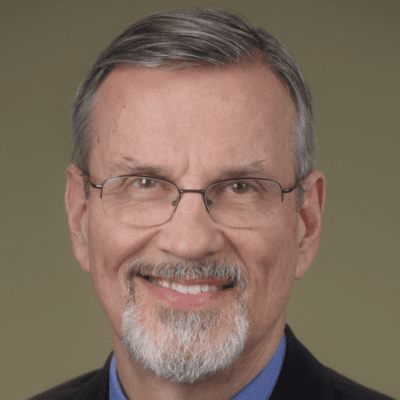
Barney S. Graham, MD, PhD, senior advisor for Global Health Equity and professor of Medicine and Microbiology, Biochemistry, and Immunology at Morehouse School of Medicine, and former deputy director of the National Institute of Allergy and Infectious Diseases (NIAID) Vaccine Research Center at the National Institutes of Health (NIH), has been selected to receive the 2022 Maxwell Finland Award for Scientific Achievement in recognition of his outstanding work in viral pathogenesis and vaccine development, culminating in the foundational discovery leading to safe and effective SARS-CoV-2 vaccines worldwide.
His innovative work on the structure of the prefusion F in respiratory syncytial virus (RSV) established a “game-changing” approach to structure-based vaccine design that is now being applied to the development of vaccines for coronaviruses and other important pathogens, including Ebola virus and influenza. Dr. Graham’s work is not only important scientifically, but continues to impact millions of lives, including the most vulnerable among us. His contributions have distinguished him as a leader in the approach to current viral pathogens and the COVID-19 pandemic, as well as a futurist in anticipating and preparing for emerging pathogens with pandemic potential.
Hear from Barney S. Graham, MD, PhD in the NFID Infectious IDeas podcast, From Early Days Farming to Pandemic Preparedness.
Tribute Video
Acceptance Speech
An Interview with Barney Graham
What is your greatest professional accomplishment?
Helping to train and inspire the next generation of researchers is my most important contribution.
Working with students and other trainees, we have focused on viral pathogenesis, immunity, and vaccine development. Our greatest accomplishment was the state of readiness we found ourselves in, when SARS-CoV-2 emerged in January 2020. Several factors made rapid COVID-19 vaccine development feasible. One was our position and resources at the NIAID Vaccine Research Center (VRC), prior experience with public health emergencies of international concern, and planning for using platform manufacturing as part of pandemic preparedness. Another was our knowledge of vaccine safety, advances in structure-based antigen design, and specific work on the structure, antigenicity, and stabilization of CoV spike. In addition, we had well-established public-private and academic collaborations that allowed us to achieve emergency use authorization of mRNA vaccines and therapeutic monoclonal antibodies in about 10 months after viral sequences became available.
What is the greatest challenge you have faced in your career?
Twice in my career, I reached a point either because of running out of research funds or an unreasonable work situation where I was close to ending my research career. In both cases, I persisted, made some high-risk choices on projects and people, and ended up with breakthroughs.
Describe a specific project or situation that has had a profound impact on you to this day.
Diagnosing and caring for one of the first AIDS patients in Tennessee when I was a chief resident at Nashville General Hospital in 1982 was a dramatic event that put me on a path to becoming a viral immunologist.
Who has had the greatest impact on your professional career development? What inspired you to work in the field of infectious diseases?
I have had many important mentors in my career, and it is hard to say who had the greatest impact. I had people during medical school and at each phase of clinical and research training at Vanderbilt, as well as an exceptional group of colleagues at the NIAID VRC who have made my career possible. If I had to choose one, it would be Anthony Fauci who had the original vision for the VRC and worked to secure the resources and support needed to function as it has. The patients I saw at Nashville General Hospital were my inspiration for working in infectious diseases.
Who do you most admire, and why?
My first was Nelson Mandela. I also have many scientific role models that I admire, but Nelson Mandela was able to change hearts and minds using truth and faith. This made a great impact on reducing social and economic disparities. Given the outcomes of the COVID-19 pandemic, I want to spend the rest of my professional time improving health equity. This means equity in who gets trained, who gets to ask the questions and do the work, and who has access to the benefits of the research.
Recognizing the challenges that we face, both as a nation and as a global community, what are the greatest threats and opportunities for the infectious disease profession?
I think the greatest threat to the infectious diseases profession is the general threat to the practice of medicine. The evolution of medicine into a profit-driven business enterprise, in my opinion, makes it harder and harder for physicians to focus on the patient and think about the biology of their disease process. The incentives are misaligned for deliberate, thoughtful patient care and lead to over-testing and emphasizing treatment above prevention of disease.
There has never been a time in my career when there was such a demand for people with expertise in infectious diseases and immunology. The pandemic revealed the threat that infectious diseases pose to humanity and there will be more opportunities for research and clinical need for trained professionals.
What are the greatest changes you have seen in the profession since you began your career?
I think the greatest change has been the ability to rapidly and specifically diagnose infectious diseases with molecular techniques. At the beginning of my fellowship, I often spent hours looking at gram stains of various tissues hoping to make a presumptive diagnosis. Now with PCR or mass spectroscopy, you can know with high specificity in a few hours. Technology advances in structural biology, protein engineering, single-cell analysis, high-throughput sequencing, and rapid chemical synthesis of nucleic acids are what made rapid COVID-19 vaccine development possible. Future technological advances will make new things possible.
Knowing what you know now, what, if anything, would you do differently in your professional life? Any regrets?
I don’t have any regrets. Looking back at all the twists and turns during my education, clinical life, scientific life, and personal life I am amazed to see how it ended up. Many of the seemingly independent threads in my life became relevant during the pandemic response. While you can see it in retrospect, it is impossible to know where each small event or experience will be woven into your life story. I believe that doing your best with whatever is in front of you at the moment will usually result in a good outcome.
What most keeps you up at night?
I sleep pretty well, but the things on my mind related to infectious diseases are how to promote action rather than just committees planning and generating documents related to pandemic preparedness. With currently existing tools, we collectively have the capability to obtain the knowledge, create the reagents, and achieve candidate vaccines, antivirals, and diagnostics for the 26 viral families prior to the next pandemic threat. This will require dedicated investigators, consistent resources, and a systematic, organized effort over several years, but is a tractable project.
What advice do you have to offer to the next generation of infectious disease professionals?
The long-standing efforts to make an HIV vaccine have led to a remarkable set of new technologies that make it possible to understand biology with a precision I could not have imagined 30 years ago. These technologies have made vaccine development more of an engineering exercise. For example, atomic level structure information allows protein engineering to create optimal vaccine antigens. Single-cell analysis provides more precise immunological endpoints and the ability to rapidly discover new human monoclonal antibodies. Rapid gene synthesis makes reagent and product development much faster. With these tools, young people should be inspired to solve many of the remaining infectious disease challenges.
Is there anything else you’d like to share?
I’ve had this quote from Teddy Roosevelt hanging in my office since I first arrived at VRC, excerpted from a speech he gave on April 23, 1910. He is one of my favorite presidents because of his efforts to reduce economic disparities:
“It is not the critic who counts … not the man who points out how the strong man stumbles or where the doer of deeds could have done better. The credit belongs to the man who is actually in the arena, whose face is marred by dust and sweat and blood, who strives valiantly, who errs and comes up short again and again, but who knows great enthusiasms, the great devotions, who, at the best knows the triumph of high achievement, and who, at the worst fails while daring greatly, so that his place shall never be with those cold and timid souls who knew neither victory nor defeat.”