The US Centers for Disease Control and Prevention (CDC) has designated November 18-24, 2013 as “Get Smart About Antibiotics Week.”
Did you know?
1. Antibiotic resistance is one of the world’s most pressing public health threats.
2. Antibiotics are the most important tool we have to combat life‐threatening bacterial diseases, but antibiotics can have side effects.
3. Antibiotic overuse increases the development of drug-resistant germs.
4. Patients, healthcare providers, hospital administrators, and policy makers must work together to employ effective strategies for improving antibiotic use–ultimately improving medical care and saving lives.
Antibiotic stewardship helps improve patient care and shorten hospital stays, thus benefiting patients as well as hospitals. In a study conducted at The Johns Hopkins Hospital, it was demonstrated that guidelines for management of community-acquired pneumonia could promote the use of shorter courses of therapy, saving money and promoting patient safety. According to a University of Maryland study, implementation of one antibiotic stewardship program saved a total of $17 million over 8 years at one institution. After the program was discontinued, antibiotic costs increased over $1 million in the first year (an increase of 23 percent) and continued to increase the following year.
The way we use antibiotics today, or in one patient, directly impacts how effective they will be tomorrow, or in another patient; they are a shared resource. Antibiotic resistance is not just a problem for the person with the infection. Some resistant bacteria have the potential to spread to others – promoting antibiotic‐resistant infections.
Targeting certain infections may decrease antibiotic use. For example, determining when and how to treat patients for urinary tract infections, the second most common bacterial infection leading to hospitalization, can lead to improved patient outcomes and cost savings.
Since it will be many years before new antibiotics are available to treat some resistant infections, we need to improve the use of antibiotics that are currently available by:
1. Ensuring all orders have dose, duration, and indications;
2. Getting cultures before starting antibiotics; and
3. Taking an “antibiotic timeout,” reassessing antibiotics after 48-72 hours.
Make appropriate antibiotic use a quality improvement and patient safety priority. Focus on reducing unnecessary antibiotic use, which can reduce antibiotic-resistant infections, Clostridium difficile infections, and costs, while improving patient outcomes. Emphasize and implement antibiotic stewardship programs and interventions for every facility – regardless of facility setting and size.
Monitor Healthcare Effectiveness Data and Information Set (HEDIS®) performance measures on pharyngitis, upper respiratory infections, acute bronchitis, and antibiotic utilization.
Visit www.cdc.gov/getsmart/healthcare/ to learn more.
Join the conversation and follow us on Twitter (@nfidvaccines), like us on Facebook, and join the NFID Linkedin Group.
Related Posts

Protecting Children as They Head Back to School
As school gets underway, experts from the National Foundation for Infectious Diseases (NFID) offer insights on childhood immunization
Lifelong Conversations about Sexual Health
Teen Health Week is April 4-10, 2022, and STD Awareness Week is April 10-16, 2022, both of which provide an opportunity for healthcare professionals to begin lifelong conversations with patients about sexual health and the importance of staying up to date on all recommended vaccines …
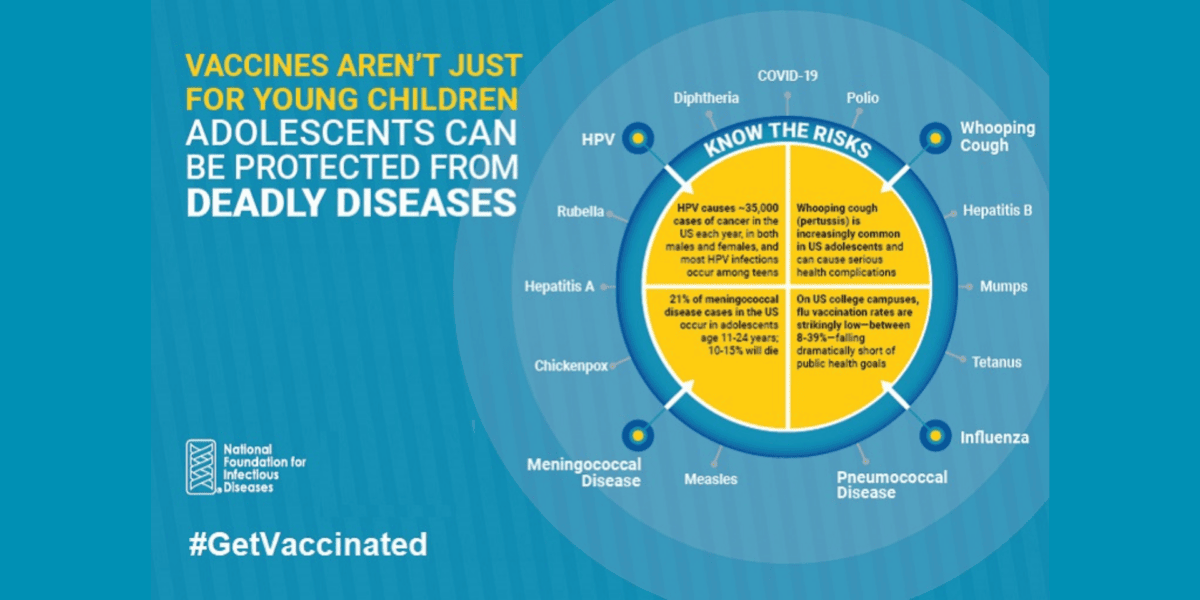
Vaccines Are Not Just for Young Children
CDC recommends vaccinations from birth to adulthood to provide a lifetime of protection. Yet many adolescents are not vaccinated as recommended, leaving them unnecessarily vulnerable. International Adolescent Health Week (March 20-26, 2022) is a perfect time to make sure that pre-teens and teens are up to date on all recommended vaccines …
