The recommendations included in this Call to Action are based on discussions at a roundtable convened by the National Foundation for Infectious Diseases (NFID) in May 2024 with representatives from more than 20 NFID partner organizations representing multidisciplinary stakeholders and subject matter experts. Discussions focused on the burden of vaccine-preventable diseases among US adults and recommendations at the healthcare system, provider, patient, and legislative/public policy levels with an overall focus on actionable and practical strategies for improving adult vaccine uptake.
Immunization substantially reduces morbidity and mortality related to vaccine-preventable diseases. However, the uptake of adult vaccines in the US is suboptimal and declining for certain vaccines and populations. Overall vaccine uptake has been negatively impacted by spillover concerns from COVID-19, as well as increasing mis- and disinformation related to vaccines. Each year, the US spends billions of dollars treating adults for diseases that could have been prevented through vaccination.
To help address this public health concern, the National Foundation for Infectious Diseases (NFID) convened a diverse group of stakeholders and experts to share observations, insights, and best practices for enhancing the uptake of all recommended adult vaccines in the US. This Call to Action highlights key outcomes of the roundtable discussions on the current state of adult immunization in the US.
Current State of Adult Immunization in the US
Impact of Vaccines on Adult Disease Burden
Vaccination is a proven, highly effective public health strategy that dramatically reduces disease burden and death (see Figure 1). For example, influenza (flu) vaccination reduces the risk of illness by 40-60% in seasons when vaccine strains are well-matched to strains in circulation.1 During the 2022-2023 flu season, vaccination prevented an estimated 5.9 million illnesses, 2.9 million medical visits, 64,000 hospitalizations, and 3,600 deaths related to influenza.2 The benefits of flu vaccination are most pronounced in adults age 50 years and older, who account for the majority of flu-related hospitalizations (approximately 70%) and deaths (more than 90%).3
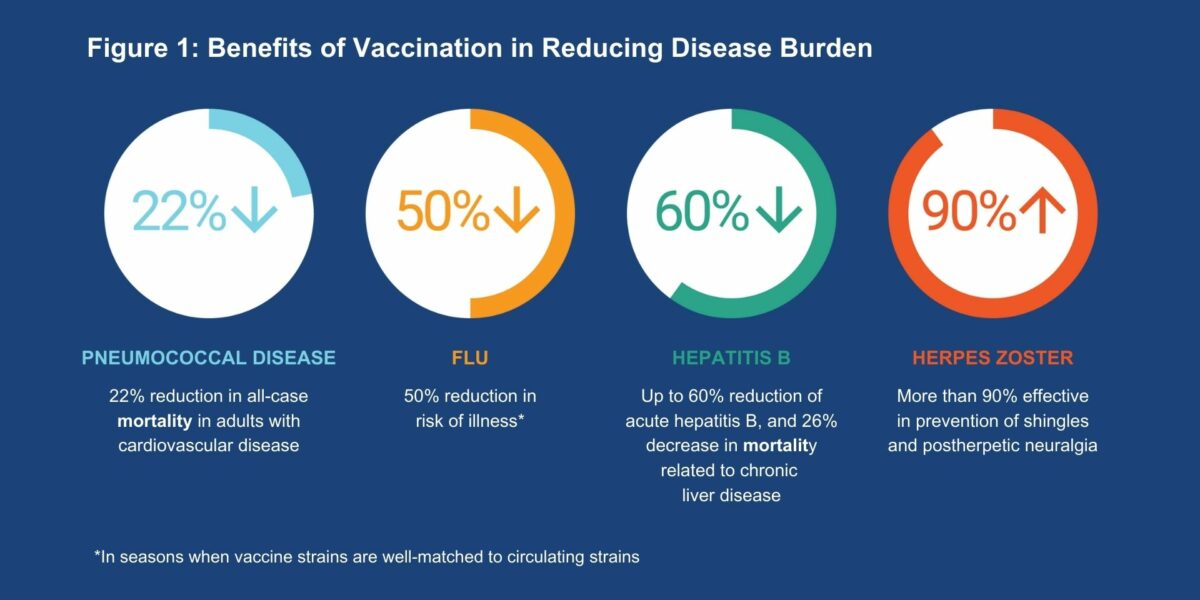
Adult immunization can also reduce morbidity and mortality related to pneumococcal disease, respiratory syncytial virus (RSV), COVID-19, and other diseases, particularly in high-risk individuals. Pneumococcal vaccination has been associated with a 22% reduction in all-cause mortality in adults with cardiovascular disease and those at high cardiovascular risk.4 Shingles vaccines available in the US, which are recommended for adults age 50 years and older, are more than 90% effective in the prevention of shingles and postherpetic neuralgia, the most common complication of the disease.5 It is estimated that, if shingles vaccine coverage reaches 65%, 4.6 million shingles cases would be prevented by the year 2032, along with 1.3 million fewer physician visits and 14,400 fewer hospitalizations.6 Hepatitis B vaccination has been associated with a 50% reduction in the rate of acute hepatitis B infection in adults,7 as well as a 26% decrease in mortality related to chronic liver disease, a 53% drop in hepatocellular carcinoma (HCC) incidence, and a 50% drop in HCC-related mortality.8
The benefits of COVID-19 vaccination have been well documented, including an estimated reduction of approximately 700,000 related hospitalizations and 120,000 deaths in the first 6 months of vaccination alone in all age groups.9 Further assessments indicate that even with limited protection against infection, vaccination can substantially mitigate COVID-19 outbreaks.10 The benefits observed to date are especially evident in adults at increased risk for COVID-19-related morbidity and mortality, including older adults, immunocompromised individuals, and those with chronic health conditions.11
Economic Considerations
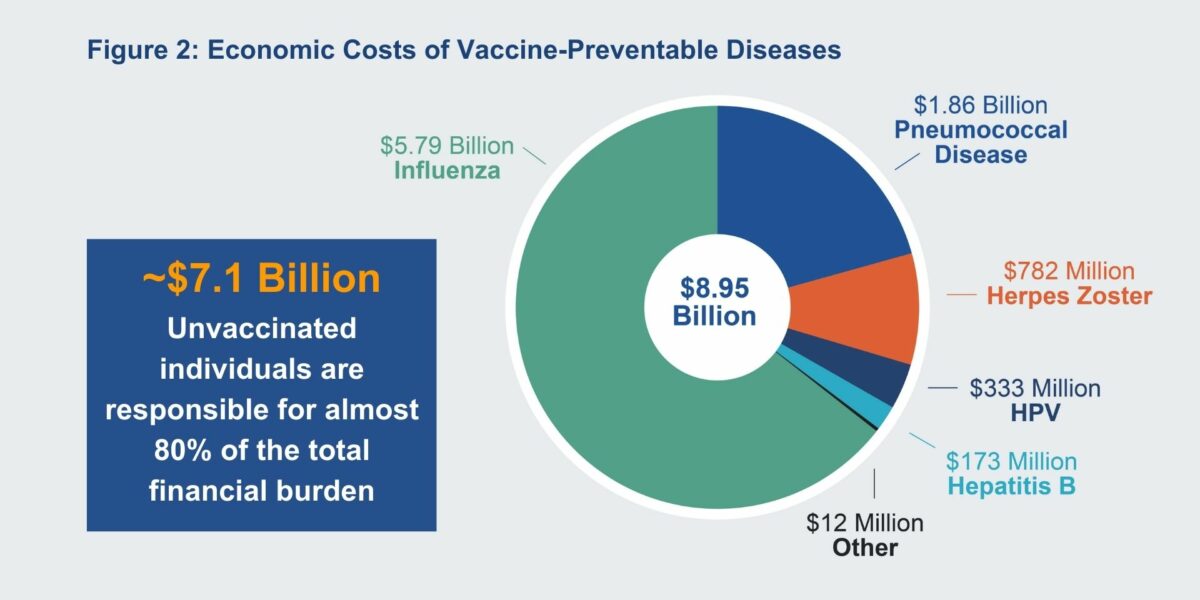
Vaccine-preventable diseases have significant economic and societal costs (see Figure 2). Vaccine coverage translates into significant cost savings for both individuals and society, with the net economic benefits of vaccination estimated at $69 billion in the United States.12 However, the economic burden of vaccine-preventable diseases remains substantial due to suboptimal immunization rates.13 The economic burden among adults can be significant, including both direct medical costs to treat and manage preventable diseases as well as indirect costs such as transportation to medical appointments and lost income due to work absences.14 According to one estimate, the US spends nearly $27 billion each year for the treatment of vaccine-preventable diseases in adults 50 and older.15 Of note, unvaccinated individuals are responsible for almost 80% of the financial burden related to vaccine-preventable diseases,16 underscoring the need to improve overall adult vaccination rates.
Declining Vaccine Coverage
Despite these benefits, US adult vaccine coverage remains low overall, with certain vaccines trending downward. Pneumococcal vaccine coverage was at its highest in 2017 and has since declined and remained relatively flat among both adults age 65 years and older as well as individuals age 18 to 64 years at increased risk. Adult flu vaccine coverage, which peaked during the 2020-2021 season, has dropped over the 2 subsequent seasons, with particularly steep declines among adults age 50-64 years as well as those age 65 years and older.
Overall vaccination rates among US adults remain concerningly low. According to recent data from the National Immunization Survey (NIS), the cumulative proportion of adults vaccinated over the preceding 9 months was below 50% for flu vaccination, and below 25% for both COVID-19 and RSV vaccines.17 Recent estimates from the Centers for Disease Control and Prevention (CDC) suggest suboptimal coverage rates and disparities in coverage for other adult vaccines including herpes zoster, hepatitis B, and tetanus.18 In 2021, overall herpes zoster vaccination coverage was 32.6% among adults age 50 years and older, with higher coverage among White adults as compared to Black and Hispanic adults. Also in 2021, hepatitis B vaccination coverage was 34.2% for adults age 19 years and older and 43.1% among travelers, both estimates lower than in 2018, with White adults again having higher coverage than Black and Hispanic adults. Tetanus vaccination (Td and Tdap) among adults age 19 years and older was 62.9% in 2019, and White adults had higher coverage compared with Black, Hispanic, and Asian adults.18
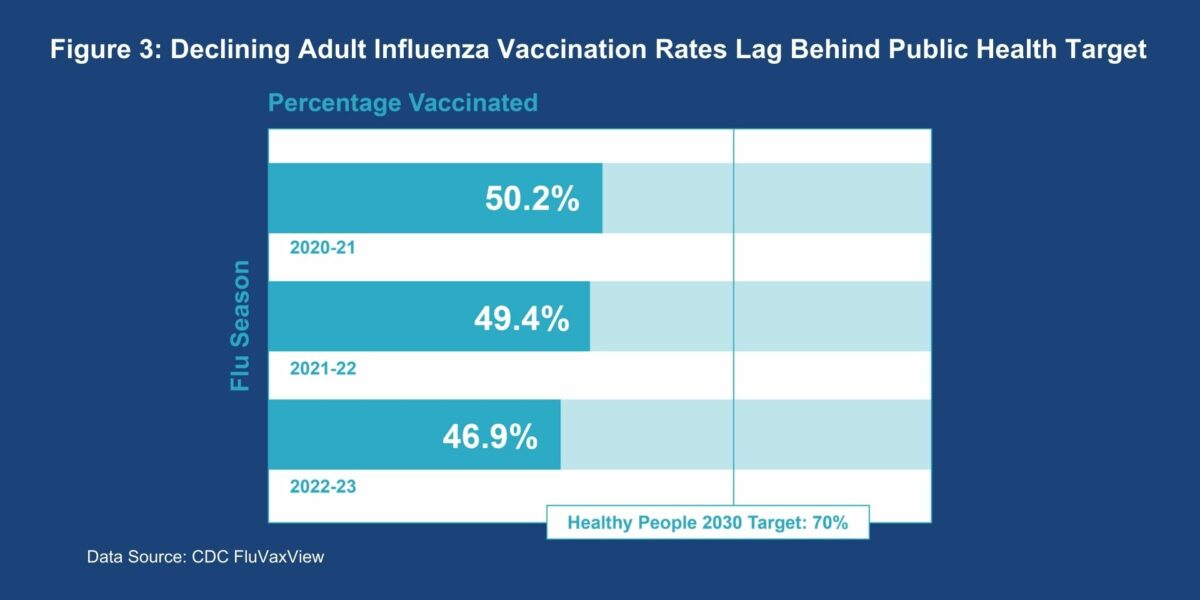
These data indicate that increasing vaccine uptake and reducing inequities in coverage remains a public health priority. The unmet need is further underscored by the failure to make progress on meeting the Healthy People 2030 goal for flu vaccine coverage: the national target of 70% flu vaccine coverage is not currently being met and is declining19 (see Figure 3). From the 2020-2021 season to the 2022-2023 season, flu vaccine coverage has dropped from 54.2% to 50.1% in adults age 50-64 years, and from 75.2% (meeting the goal) to 69.7% (missing the goal) in adults age 65 years and older.20 These coverage deficits are especially concerning given that, due to the demographics of an aging population, the health burden of flu and other vaccine-preventable diseases is expected to increase in coming years.21
Disparities in Immunization Rates
Improvements in adult vaccine uptake could provide an even greater impact on public health in certain populations. This includes at-risk groups such as older adults, immunocompromised patients, and those with chronic health conditions, as well as racial and ethnic groups in which disparities have been observed. Several key examples include:
- Influenza (flu): In 2022-2023, flu vaccine coverage was only about 70% in adults age 65 years and older—the largest growing demographic in the US—and just 55% in adults age 50-64 years.3 While younger adults age 18-49 years are generally at lower risk, flu vaccine coverage in this group was approximately 44% in 2022-2023,3 suggesting a missed opportunity to make annual vaccination a routine part of healthcare while adults are relatively younger, healthier, and at lower risk of adverse flu-related outcomes. Inequities are also evident among certain racial/ethnic groups. For example, during the 2022-2023 season, flu vaccine uptake was 51% among White and Asian adults, but just 43% among Black adults and 37% among Hispanic and American Indian and Alaska Native (AI/AN) adults.22
- Pneumococcal: According to data from the 2021 National Health Interview Survey,23 vaccination coverage (≥1 dose of any type of pneumococcal vaccine) was 22.2% for adults age 19-64 years at increased risk for pneumococcal disease and coverage was lower among Hispanic (19%) and Asian (16.9%) adults compared to White adults (23.3%). Among adults age 65 years and older, vaccine coverage was 65.8%, including 70.1% among White individuals, compared to Hispanic (46.2%), Black (54.8%), and Asian (55.8%) individuals.23
- Herpes zoster (shingles): Coverage (≥1 dose of any type of herpes zoster vaccination) in 2021 was only 32.6% for adults age 50 years and older, and 41.1% for adults age 60 years and older. Similar to pneumococcal vaccine, coverage rates were lower in Black and Hispanic adults compared to White adults.23
Factors Contributing to Suboptimal Vaccination Rates
- Access and equity issues: The COVID-19 pandemic clearly highlighted disparities in vaccination rates by race, ethnicity, income level, insurance status, and geography.24 However, equity in vaccine access remains an important issue that has not been resolved, and is exacerbated by geographic, financial, cultural, and access barriers among others.
- For adults age 65 years and older, many recommended vaccines are allocated to Medicare Part D, and pharmacists are the major administrators of vaccines to this population.
- Point-of-care vaccination in medical clinics can be an effective means of increasing vaccination rates, especially among patients with high-risk conditions (e.g., cancer) who require special vaccination schedules. Some providers find it difficult to administer and be reimbursed for Part D-covered vaccines.
- While pharmacists play a significant role in administering adult vaccines, and are an ideal access point for adult vaccines including herpes zoster,25 laws governing administration of vaccines by pharmacists are inconsistent, varying from state to state.26 Pharmacists may face barriers to providing vaccination, including lack of staff to manage and administer vaccines, inadequate reimbursement, and being an out-of-network provider.27
- Economic impacts: Funding mechanisms for vaccines can be complex and difficult to navigate for healthcare professionals and patients alike. A substantial proportion of US adults lack insurance coverage for some recommended vaccines. For healthcare professionals, reimbursement rates vary widely across the US and in some states, Medicare reimbursement levels may be insufficient to cover costs, which may hinder equitable vaccine uptake.28 Additionally, Medicaid reimbursement for adult vaccinations (including administration fees) differs by state, adding to the challenge.
- Engagement of healthcare professionals: A strong vaccine recommendation from a healthcare professional has the biggest impact on patient acceptance, yet in many cases, the recommendations are weak or nonexistent. Healthcare professionals may not give strong vaccine recommendations for a number of reasons, including time constraints (limited time available for an individual patient encounter), competing priorities (addressing health conditions perceived as more critical to patient health), lack of vaccine knowledge, or even personal beliefs or concerns about vaccines that may temper their willingness to recommend vaccines.29 Team-based approaches and standing orders authorizing immunization can enhance vaccination rates, but to be most effective, these strategies must be accompanied by training and education as well as a strong recommendation from a healthcare professional.
- Limited awareness: Adults are often unaware of all vaccine recommendations, and documentation of immunization histories are inconsistent. Additionally, many healthcare professionals are unaware of updated vaccination guidelines for adults.30 Frequently changing guidelines and misunderstandings about vaccine “seasonality” also detract from optimal adult vaccination rates.
- Increasing complexity: Vaccine schedules can be confusing for patients and healthcare professionals. The current US adult vaccine schedule includes 15 vaccine categories, with recommendations that vary by patient status including pregnancy, immunocompromised, and chronic health conditions such as diabetes, heart disease, and lung disease.31 Posing further challenges is that immunocompromised patients and those with certain chronic health conditions (e.g., kidney disease) are heterogeneous populations that often require further specificity within the schedule. This complexity will likely increase as additional vaccines are introduced. By one estimate, the number of diseases covered in the adult vaccine landscape could triple within the next 5 years, with a commensurate increase in the number of approved vaccines.21
- Healthcare system challenges: The delivery system is complex in terms of the infrastructure and logistics needed to effectively distribute and administer vaccines. Coordination between healthcare professionals, including pharmacies and primary care, can be difficult due to incomplete patient immunization histories and inconsistencies in data tracking. All state and local immunization information systems (IIS) or registries can record adult vaccinations; however, not all providers submit data to IIS, in part due to the high cost of creating interfaces and the time and resources required for data entry. Additionally, data is not easily exchanged between systems primarily due to policies limiting data sharing, and even within structured interfaces there may be data quality issues in reporting between EMR systems and registries.
- Insufficient public health funding at both state and federal levels: Chronic underfunding of the US public health system predated the COVID-19 pandemic and made the US more susceptible to COVID-19 deaths and disruptions compared to other industrialized countries. Funding to support public health preparedness in states has declined by 25% over the last 2 decades—about 50%, accounting for inflation. This level of shortfall leaves little room for innovation, flexibility, and modernization.32
- Vaccine hesitancy and misinformation: Anti-vaccine narratives are not new, but the way they spread has changed radically. Today, false information online reaches people 6 times faster than factual information and is 70% more likely to be shared.33 The legacy of the COVID-19 pandemic is an increase in vaccine misinformation, disinformation, anti-vaccine propaganda, and viral rumors that continue to negatively impact vaccine uptake. Anti-vaccine narratives continue to proliferate, decreasing trust and confidence in institutions and healthcare professionals, polarizing the public, and detracting from evidence-based vaccine safety/efficacy information. Viral content is often driven by influencers who are highly trusted by their followers. 34
The pandemic did have a positive effect on vaccine acceptance including a better understanding among older adults of how and where to get vaccinated. Additionally, an important post-pandemic change in public perception of vaccination is an increasing awareness that, although vaccination does not completely prevent infection in all patients, vaccination can help protect against serious outcomes, including hospitalization and death.
Recommendations for Improving Adult Immunization Uptake
Roundtable participants emphasized the need to optimize adult vaccination uptake using practical strategies. The recommendations focus on the following areas:
Healthcare System Strategies
- Improve and enhance IIS: Registries are important to accurately document vaccinations and identify coverage gaps.35 It is critical that these systems capture data on all adult vaccinations, including those given in pharmacies. Electronic patient and health management systems should be seamlessly integrated with IIS to exchange records for every patient at every visit, helping to ensure accurate patient vaccination history evaluation and recommendations. As there is currently no national system, work should be done to bridge gaps in interoperability between IIS, balancing the needs of individual states with the overarching need for a streamlined and collaborative national approach. Finally, the challenges faced by individual states must be addressed, as states may have funding challenges and may not prioritize the development and maintenance of information systems due to competing public health priorities.
- Ensure awareness and understanding of adult vaccine recommendations among all healthcare professionals: Centralized platforms should be leveraged to increase awareness and ensure that the recommended adult vaccine schedule reaches a broad audience quickly and efficiently. Primary care professionals, specialists, and those providing inpatient care often receive practice-specific information from their respective professional societies, making these organizations highly influential and important as a channel for disseminating new and revised guidelines.
- Link performance to vaccination: Opportunities exist to explore the introduction of new performance measures in hospitals and health systems while aligning healthcare professional compensation with performance on vaccination metrics.
- Leverage technology: Patient education and follow-up can be improved with technology. Digital tools can be used to push out vaccination reminders and supporting messages. Multiple communication channels should be leveraged (including email, text, and phone notifications) to account for varying communication preferences. Electronic health record (EHR) prompts can be enhanced with reminders and recall notifications to ensure that recommended vaccinations are delivered on a timely basis. EHRs and IIS can also be used to provide patients with access to their vaccination records.
- Utilize combination vaccines and new technology platforms: Increasing confusion over the adult vaccine schedule may be mitigated by formulations combining multiple vaccines into one administration, through combination vaccines. Although only a few are currently approved for adults, novel combination vaccines in development could help facilitate timely vaccination, lower costs for shipping and stocking, and may reduce the number of vaccination-related healthcare visits. Cold chain and vaccine stability issues are also important considerations for implementation of immunization outreach in rural communities, workplaces, and other non-traditional venues. Stakeholders should prepare by considering key questions regarding vaccine approval, guidelines, uptake, and mechanisms for reimbursement.36 Additionally, needle-free technologies and self-administered vaccines in development may help increase adult immunization rates among those who are needle-phobic or those who have access issues.
Healthcare Professional Strategies
- Simplify vaccine recommendations: To enhance vaccine uptake, vaccine recommendations should be specific, streamlined, and personalized to the individual patient.
- Emphasize the importance of healthcare professional endorsement: A strong healthcare professional recommendation to vaccinate is one of the best predictors of vaccine acceptance and coverage.37 Healthcare professionals are a credible and trusted source for patient information and decision-making support. Accordingly, healthcare professionals should be trained on how to provide strong recommendations to position vaccination as an integral part of patient management, especially for high-risk adult patients. Additional training on motivational interviewing when encountering patient reluctance is also a critical factor for success.
- Broaden specialist outreach: Specialists (including cardiologists, OB/GYNs, oncologists, pulmonologists, and others) should be prepared to integrate vaccination protocols into clinical practice to prevent complications in adults with chronic health conditions. Medical societies should consider issuing vaccine-specific guidelines (or updating disease-specific guidelines with sections on vaccination) to help healthcare professionals better understand how vaccine strategies for patients with comorbid conditions may differ from those for healthy adults.38 Ongoing vaccine training should be required for all healthcare professionals, regardless of specialty, to help improve patient outcomes. Furthermore, education about vaccines should be included in the curriculum of all specialty and subspecialty training programs, and certification exams should include questions on vaccines to ensure that specialists are well-prepared to support immunization efforts.
- Address disparities: Partnerships should be built with healthcare professionals to increase understanding of the unique needs and barriers to vaccination in diverse populations. Enlisting trusted community leaders to advocate for vaccines and boost confidence and uptake can also help reduce health disparities.39
- Expand clinical support for vaccination: Every medical visit is an opportunity to discuss and recommend vaccinations. All staff should be empowered to recommend vaccination at each point of patient contact (and provide documentation and follow-up when vaccination is declined). Co-administration of vaccines can be encouraged when appropriate (e.g., influenza and COVID-19 vaccines). In addition, healthcare professionals should be educated on best practices for immunization, including safe and effective techniques to avoid discomfort and prevent vaccine-related injuries.40
Patient Strategies
- Develop messaging to address common post-pandemic concerns:
- Concerns about the accelerated development and approval of COVID-19 vaccines may extend to other vaccines. Messages (to both the public and healthcare professionals) should focus on the safety and efficacy of recommended vaccines and the comprehensive, robust US systems in place to monitor safety on an ongoing basis. Messaging on the importance of protecting the family may resonate with vaccine-hesitant individuals.
- Messaging needs to be consistent, simplified for the general public, culturally and linguistically relevant, and delivered at all points of patient contact.
- Resources including responses to frequently asked questions can help manage misinformation about vaccination by directly addressing specific concerns.
- Misinformation can also be addressed by “message ambassadors” trained to deliver key messages on vaccination to targeted groups. Healthcare professionals (including nurses, physicians, and pharmacists) as well as scientists are often considered credible ambassadors, and interactions with them have been shown to increase vaccine confidence. By contrast, messages perceived as coming from government officials may increase resistance to vaccination among the vaccine-hesitant and skeptical.
- Needle anxiety is reported to be a reason for non-vaccination in approximately 10% of individuals. Healthcare professionals should be aware of safe, effective, and practical steps that can be taken to reduce vaccination-related pain and anxiety.41
- Customize messaging: Messages supporting vaccination should be tailored for specific communities. Efforts are needed to address concerns of specific age groups, including older adults, and populations including patients who are immunocompromised and those with chronic health conditions. Across at-risk populations, messages should focus on vaccination as a proven strategy to decrease the severity of disease and the risk for hospitalization.42
- Vaccinate people where they are: To improve accessibility, vaccinations must be delivered where people live and work. Access can be improved by supporting vaccination at accessible locations beyond medical offices and hospitals, including pharmacies, workplaces, schools/universities, and when possible, at home.
- Implement advanced marketing tactics: Proactive public outreach to patients and caregivers through social media can amplify public health messages where patients are primed to receive them.
- Mobilize the community to address vaccine awareness, affordability, and access: New programs are needed that address vaccine affordability for individuals without insurance coverage and/or access to venues for vaccination. Successful programs related to improving access have included training of vaccine ambassadors who are trusted by the community and can deliver education at sites known and valued by target audiences.
Legislative and Public Policy Initiatives
- Advocate for funding: Immunization infrastructure can be improved by strengthening and sustaining funding for a national immunization program.43 Funding is needed to support state and local immunization programs to increase vaccination rates overall, and in underserved populations, as well as for surveillance, outbreak response, vaccine education, and information system improvements.32
- Endorse legislative and public policy initiatives: The proposed Vaccines for Adults program will support systems and strategies for hard-to-reach and vaccine hesitant populations.43 This program would improve both vaccine access and uptake by covering all recommended vaccines at no cost for uninsured adults.44
- Reduce or eliminate financial barriers to vaccination: Recent changes in Medicare/Medicaid policies have reduced some of the financial burden and have eliminated copays and out-of-pocket expenses for recommended adult vaccines.45 However, there are still coverage gaps for uninsured adults, and efforts are needed to address these gaps and ensure that uninsured and under-insured individuals have access to all recommended vaccines.43
Conclusion
Increasing the proportion of adults who receive recommended vaccines continues to be a high-priority public health issue.23 Improving adult immunization rates in the US requires a multi-faceted strategy involving health system improvements, public health initiatives, and community outreach. This Call to Action aims to raise awareness about the impacts of suboptimal adult vaccine coverage, highlight the complex challenges and barriers to improving vaccine uptake, and promote promising practical approaches to overcoming these challenges. Through coordinated efforts, we can improve adult immunization coverage and reduce the burden of vaccine-preventable diseases, leading to overall improvements in public health.
Partner Organizations
AARP
Adult Vaccine Access Coalition
Alliance for Aging Research
Alliance for Patient Access
American Academy of Family Physicians
American Association of Nurse Practitioners
American College of Obstetricians and Gynecologists
American College of Preventive Medicine
American Heart Association
American Immunization Registry Association
American Lung Association
American Pharmacists Association
American Public Health Association
American Society of Clinical Oncology
AMGA
Association for Professionals in Infection Control and Epidemiology
Association of Immunization Managers
Association of State and Territorial Health Officials
Centers for Disease Control and Prevention
Fred Hutchinson Cancer Center
Gerontological Society of America
Good Health WINs/National Council of Negro Women
Immunize.org
National Adult and Influenza Immunization Summit
National Alliance for Hispanic Health
National Association of Community Health Centers
National Foundation for Infectious Diseases (NFID)
National Medical Association
National Minority Quality Forum
Unbiased Science
Support
This activity is sponsored by NFID with support through unrestricted educational grants from GSK, Merck & Co., Inc., ModernaTX, Inc., Pfizer Inc., and Sanofi Pasteur Inc. NFID policies prohibit funders from controlling program content.
References
1. Trombetta CM, Kistner O, Montomoli E, Viviani S, Marchi S. Influenza Viruses and Vaccines: The Role of Vaccine Effectiveness Studies for Evaluation of the Benefits of Influenza Vaccines. Vaccines (Basel). 2022;10(5).
2. Centers for Disease Control and Prevention. Past Seasons Burden Prevented Estimates. Last Reviewed: December 29, 2023. www.cdc.gov/flu/vaccines-work/past-burden-prevented-est.html.
3. Centers for Disease Control and Prevention. Estimated Influenza Illnesses, Medical Visits, Hospitalizations, and Deaths Prevented by Vaccination in the United States – 2022-2023 Influenza Season. Last Reviewed: December 13, 2023. www.cdc.gov/flu/about/burden-prevented/2022-2023.htm.
4. Marques Antunes M, Duarte GS, Brito D, et al. Pneumococcal vaccination in adults at very high risk or with established cardiovascular disease: systematic review and meta-analysis. European Heart Journal – Quality of Care and Clinical Outcomes. 2020;7(1):97-106.
5. Centers for Disease Control and Prevention. What Everyone Should Know about the Shingles Vaccine (Shingrix). Last reviewed May 8, 2023. www.cdc.gov/vaccines/vpd/shingles/public/shingrix/index.html.
6. Patterson BJ, Buck PO, Curran D, et al. Estimated Public Health Impact of the Recombinant Zoster Vaccine. Mayo Clinic Proceedings: Innovations, Quality & Outcomes. 2021;5(3):596-604.
7. Hunter P, Fryhofer SA, Szilagyi PG. Vaccination of Adults in General Medical Practice. Mayo Clin Proc. 2020;95(1):169-183.
8. Chiang C-J, Jhuang J-R, Yang Y-W, et al. Association of Nationwide Hepatitis B Vaccination and Antiviral Therapy Programs With End-Stage Liver Disease Burden in Taiwan. JAMA Network Open. 2022;5(7):e2222367-e2222367.
9. Yamana TK, Galanti M, Pei S, et al. The impact of COVID-19 vaccination in the US: Averted burden of SARS-COV-2-related cases, hospitalizations and deaths. PLoS One. 2023;18(4):e0275699.
10. Moghadas SM, Vilches TN, Zhang K, et al. The impact of vaccination on COVID-19 outbreaks in the United States. medRxiv. 2021.
11. Moss P, Berenbaum F, Curigliano G, Grupper A, Berg T, Pather S. Benefit-risk evaluation of COVID-19 vaccination in special population groups of interest. Vaccine. 2022;40(32):4348-4360.
12. Orenstein WA, Ahmed R. Simply put: Vaccination saves lives. Proc Natl Acad Sci U S A. 2017;114(16):4031-4033.
13. Kolobova I, Nyaku MK, Karakusevic A, Bridge D, Fotheringham I, O’Brien M. Burden of vaccine-preventable diseases among at-risk adult populations in the US. Hum Vaccin Immunother. 2022;18(5):2054602.
14. Talbird SE, La EM, Carrico J, et al. Impact of population aging on the burden of vaccine-preventable diseases among older adults in the United States. Hum Vaccin Immunother. 2021;17(2):332-343.
15. McLaughlin JM, McGinnis JJ, Tan L, Mercatante A, Fortuna J. Estimated Human and Economic Burden of Four Major Adult Vaccine-Preventable Diseases in the United States, 2013. J Prim Prev. 2015;36(4):259-273.
16. Ozawa S, Portnoy A, Getaneh H, et al. Modeling The Economic Burden Of Adult Vaccine-Preventable Diseases In The United States. Health Aff (Millwood). 2016;35(11):2124-2132.
17. Centers for Disease Control and Prevention. Vaccination Trends – Adults. Data as of: 07/04/2024. www.cdc.gov/respiratory-viruses/data-research/dashboard/vaccination-trends-adults.html.
18. Centers for Disease Control and Prevention. Vaccination Coverage among Adults in the United States, National Health Interview Survey, 2021. Last reviewed July 19, 2023. www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/vaccination-coverage-adults-2021.html
19. Healthy People 2030. Objective: Increase the proportion of people who get the flu vaccine every year — IID‑09. https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-people-who-get-flu-vaccine-every-year-iid-09.
20. Centers for Disease Control and Prevention. FluVaxView Interactive. Last reviewed May 28, 2021. www.cdc.gov/flu/fluvaxview/interactive-general-population.htm.
21. Jones CH, Jenkins MP, Adam Williams B, Welch VL, True JM. Exploring the future adult vaccine landscape—crowded schedules and new dynamics. npj Vaccines. 2024;9(1):27.
22. Centers for Disease Control and Prevention. Health Equity and Flu. Last reviewed March 21, 2024. www.cdc.gov/flu/highrisk/disparities-racial-ethnic-minority-groups.html.
23. Hung M-C, Srivastav A, Lu P-J, et al. Vaccination Coverage among Adults in the United States, National Health Interview Survey, 2021. AdultVaxView. Last Reviewed: July 19, 2023. www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/vaccination-coverage-adults-2021.html.
24. National Center for Immunization and Respiratory Diseases. COVID-19 Vaccine Uptake and CDC’s Commitment to Vaccine Equity. November 22, 2023. www.cdc.gov/ncird/whats-new/vaccine-equity.html.
25. Tak CR, Marciniak MW, Savage A, Ozawa S. The essential role of pharmacists facilitating vaccination in older adults: the case of Herpes Zoster. Hum Vaccin Immunother. 2020;16(1):70-75.
26. DeMaagd G, Pugh A. Pharmacists’ Expanding Role in Immunization Practices. October 18, 2023. www.uspharmacist.com/article/pharmacists-expanding-role-in-immunization-practices.
27. Srivastav A, Black CL, Lutz CS, et al. U.S. clinicians’ and pharmacists’ reported barriers to implementation of the Standards for Adult Immunization Practice. Vaccine. 2018;36(45):6772-6781.
28. Polaris JJZ, Eiden AL, DiFranzo AP, Pfister HR, Itzkowitz MC, Bhatti AA. State Medicaid Coverage and Reimbursement of Adult Vaccines Administered by Physicians and Pharmacists. AJPM Focus. 2024;3(4).
29. Prieto-Campo Á, Batista AD, Magalhães Silva T, et al. Understanding vaccination hesitation among health professionals: a systematic review of qualitative studies. Public Health. 2024;226:17-26.
30. Infectious Diseases Society of America. Adult Immunization: Shots to Save Lives. February 2010. www.idsociety.org/globalassets/idsa/policy–advocacy/current_topics_and_issues/immunizations_and_vaccines/statements/adult-immunization–shots-to-save-lives-pdf.
31. Centers for Disease Control and Prevention. Recommended Adult Immunization Schedule. June 27, 2024. www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf.
32. Trust for America’s Health. The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022. July 2022. www.tfah.org/wp-content/uploads/2022/07/2022PublicHealthFundingFINAL.pdf.
33. Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. 2018;359(6380):1146-1151.
34. Samuels E, Kelly M. How false hope spread about hydroxychloroquine to treat covid-19—and the consequences that followed. April 13, 2020. www.washingtonpost.com/politics/2020/04/13/how-false-hope-spread-about-hydroxychloroquine-its-consequences/.
35. Centers for Disease Control and Prevention. Immunization Information Systems (IIS). Last Reviewed: September 28, 2023. www.cdc.gov/vaccines/programs/iis/index.html.
36. Avalere. Adult Seasonal Combination Respiratory Vaccines: Policy Considerations. May 2024. https://avalere.com/wp-content/uploads/2024/05/White-Paper_Adult-Seasonal-Combination-Respiratory-Vaccines-Policy-Considerations-.pdf.
37. Dudley MZ, Schuh HB, Forr A, Shaw J, Salmon DA. Changes in vaccine attitudes and recommendations among US Healthcare Personnel during the COVID-19 pandemic. npj Vaccines. 2024;9(1):49.
38. Kamboj M, Bohlke K, Baptiste DM, et al. Vaccination of Adults With Cancer: ASCO Guideline. Journal of Clinical Oncology. 2024;42(14):1699-1721.
39. National Foundation for Infectious Diseases. 4 Ways to Address Disparities in Vaccination Rates. April 29, 2024. www.nfid.org/4-ways-to-address-disparities-in-vaccination-rates/.
40. Bancsi A, Houle SKD, Grindrod KA. Shoulder injury related to vaccine administration and other injection site events. Can Fam Physician. 2019;65(1):40-42.
41. Immunize.org. Improving the Vaccination Experience. www.immunize.org/clinical/vaccine-confidence/topic/improving-vaccine-experience/. Accessed August 21, 2024.
42. Merschel M. What people with heart disease should know about vaccines today. October 6, 2023. www.heart.org/en/news/2023/10/06/what-people-with-heart-disease-should-know-about-vaccines-today.
43. NCIRD Immunizations. Immunizations and Vaccines for Adults. Updated April 17, 2023. www.cdc.gov/budget/documents/fy2024/Immunizations-Vaccines-Factsheet.pdf.
44. Johns M. The U.S. Needs a Federal Program To Expand Vaccine Access and Equity for Adults. April 18, 2023. www.americanprogress.org/article/the-u-s-needs-a-federal-program-to-expand-vaccine-access-and-equity-for-adults/.
45. Sayed BA, et al. Medicare Part D Enrollee Vaccine Use After Elimination of Cost Sharing for Recommended Vaccines in 2023. May 3, 2024. https://aspe.hhs.gov/sites/default/files/documents/3854c8f172045f5e5a4e000d1928124d/part-d-covered-vaccines-no-cost-sharing.pdf.
Download Poster Presentation: Strategies to Improve Adult Immunization in the US
Related Resources

Adult Vaccine Resources
Videos, graphics, and social media posts to help raise awareness about the importance of adult vaccination

Preventable Problems
Life is full of unavoidable challenges—but some are preventable. Staying up to date on all recommended vaccines helps protect you and those you care about from serious diseases.

One Thing We Can Agree On
We may not agree on everything, but we can all agree that protecting our health is essential. Millions of adults in the US get sick each year from preventable diseases. The good news? Vaccines and healthy habits can help protect us all.