
Special thanks to NFID Director Sara E. Cosgrove, MD, MS, professor of medicine at Johns Hopkins University School of Medicine and director of the Johns Hopkins Hospital Department of Antimicrobial Stewardship, for this guest blog post on the importance of antibiotic stewardship, even during a pandemic. November 18-24, 2022, is US Antibiotic Awareness Week, an annual observance to raise awareness of the threat of antibiotic resistance and the importance of appropriate antibiotic use.
As if the impacts of the global COVID-19 pandemic were not bad enough, according to a special report from the Centers for Disease Control and Prevention (CDC), the threat of antimicrobial-resistant infections is not only still present, but has become even more prominent. CDC found that during the first year of the COVID-19 pandemic, more than 29,400 people in the US died from antimicrobial-resistant infections. Of these, nearly 40% got the infection while they were in the hospital.
As a hospital-based infectious disease physician, I know it can be hard to determine whether patients hospitalized with COVID-19 are ill because of COVID-19 or because of super infection with resistant organisms. Many patients who died with resistant organisms also had very severe lung disease due to COVID-19. At Johns Hopkins, I saw a pathology specimen of an infected lung that looked like a liver, with no air spaces visible. It is not surprising that extremely sick, hospitalized patients whose lungs were not healing were treated with multiple courses of antibiotics. It is hard to watch a hospitalized patient get very sick with pneumonia and not prescribe an antibiotic, even if the pneumonia is most likely caused by a viral infection like COVID-19.
The pandemic created a perfect storm for resistant organisms to flourish: COVID-19 disease caused surges in hospitalization with a proportion of patients experiencing severe disease that led to prolonged hospitalization and the use of invasive medical devices such as central catheters and mechanical ventilation. At the same time, the pandemic also diminished the ability of hospitals to perform optimal infection prevention and antibiotic stewardship activities because staff and resources were diverted to COVID-19 response. Many hospitals have experienced enormous attrition of infection control professionals and antibiotic stewards due to exhaustion, which still haunts us.
If a surge in respiratory infections occurs again—as is currently happening in some areas of the US—hospitals and nursing homes must continuously support strong infection prevention and stewardship programs in order to mitigate the damage from antibiotic resistance.
But combating antibiotic resistance is not just a job for healthcare professionals—it is everyone’s responsibility. We need to build health literacy about antibiotics among prescribers and patients alike.
Antibiotics should only be used for bacterial infections, not viruses. As a physician, I try to help people understand that the human body is full of bacteria, so when you take an antibiotic there is a good chance that the “good” bacteria in your gut will become more resistant to that antibiotic. Some people will not have consequences from this, but others will develop subsequent resistant infections or pass resistant bugs on to family members. Further, antibiotics have side effects. Some, like mild rashes, stomach upset, diarrhea, and yeast infections, are simply inconvenient and annoying. Others, such as Clostridioides difficile (C. diff) infection and severe skin rashes, can be serious and may need medical attention. So why take an antibiotic if it is not going to help but could cause resistance and side effects?
As a mom, I practice what I preach. My 18-year-old daughter has never had a single antibiotic. My 16-year-old son has had only one dose before a surgical procedure.
 The global experience with COVID-19 should impact our thinking about respiratory viruses. Giving consumers easy access to COVID-19 testing likely mitigated some, but certainly not all, requests for unnecessary antibiotics.
The global experience with COVID-19 should impact our thinking about respiratory viruses. Giving consumers easy access to COVID-19 testing likely mitigated some, but certainly not all, requests for unnecessary antibiotics.
We need to empower people to recognize a respiratory virus and have a plan for how to deal with it. If you have a stuffy or runny nose, sore throat, cough, headache, and muscle aches, it is probably due to a virus—which means an antibiotic will not help.
We all need to develop a stewardship mindset. Antibiotics are incredibly valuable, but only when used as needed to treat bacterial infections.
In my experience, patients who ask for antibiotics are usually seeking reassurance and symptomatic improvement. We need to do a better job of educating the public about colds—if you want to stay healthy, wash your hands, cover your coughs and sneezes, get plenty of sleep, and make sure everyone in your family is up to date on all recommended vaccines. If you do get sick, not only should you stay home, but take a day to rest and recover—just because you can tune in to another Zoom meeting from home, does not mean you should. Make sure you have a supply of things like ibuprofen, acetaminophen, tea and honey, throat lozenges, and decongestants that can help relieve symptoms.
We must all act on the lessons learned from COVID-19: When you have respiratory symptoms, get tested. A test can determine whether it is a virus such as COVID-19 or influenza (flu), both of which can be treated with antivirals (but not antibiotics).
We all need to develop a stewardship mindset. Antibiotics are incredibly valuable, but only when used as needed.
Take the Antibiotic Stewardship Pledge
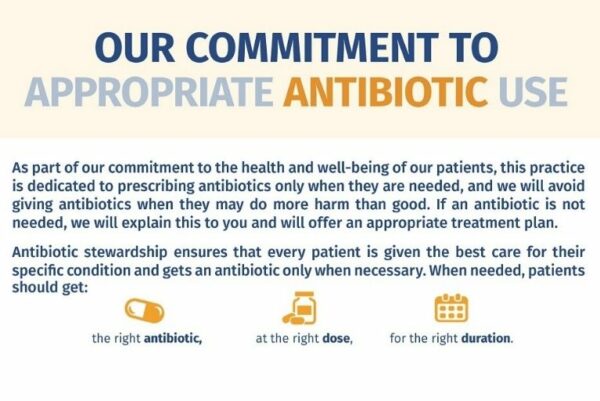 Download and share the NFID Antibiotic Stewardship Pledge to show your commitment to reducing antibiotic resistance through appropriate antibiotic use.
Download and share the NFID Antibiotic Stewardship Pledge to show your commitment to reducing antibiotic resistance through appropriate antibiotic use.
To join the conversation and get the latest news on infectious diseases, follow NFID on Twitter using the hashtag #BeAntibioticsAware, like NFID on Facebook, follow NFID on Instagram, visit NFID on LinkedIn, and subscribe to receive future NFID Updates.
Related Posts

5 Things To Know about Antibiotic Resistance
There are steps everyone can take to help protect against drug-resistant infections
C. diff: An Urgent Public Health Threat
November is C. diff Awareness Month, an annual opportunity to raise awareness about this common but potentially deadly infection
Thank You for Appropriately Using Antibiotics
Special thanks to NFID Director S. Shaefer Spires, MD, of Duke University Hospital for this guest blog post for US Antibiotic Awareness Week (November 18-24, 2021), an annual observance to raise awareness of the threat of antibiotic resistance and the importance of appropriate antibiotic use …
