Almost all cervical cancer in the US is caused by human papillomavirus (HPV). January is Cervical Health Awareness Month—a timely reminder about the importance of getting vaccinated against HPV.
1. HPV vaccination is cancer prevention
 HPV can cause cervical cancer as well as other genital, mouth, and throat cancers. HPV causes many pre-cancerous cervical lesions that may need surgery. HPV vaccination can help protect against several types of cancer, including oropharyngeal (throat) cancer which is more common in men.
HPV can cause cervical cancer as well as other genital, mouth, and throat cancers. HPV causes many pre-cancerous cervical lesions that may need surgery. HPV vaccination can help protect against several types of cancer, including oropharyngeal (throat) cancer which is more common in men.
Each year in the US:
- More than 4,000 women die from cervical cancer
- More than 20,000 women and more than 15,000 men are affected by cancers caused by HPV
Before HPV vaccines were introduced, roughly 340,000-360,000 women and men saw a healthcare professional for management of genital warts caused by HPV every year.
2. HPV is very common
HPV is so common that almost every sexually active person will get an HPV infection at some point in their life. There are an estimated 14 million new cases in the US annually. Most new infections are in individuals in their teens and early 20s. HPV vaccination can prevent most of those infections, including approximately 90% of those that can lead to cancer.
The Centers for Disease Control and Prevention (CDC) estimates that there were 43 million HPV infections in the US in 2018, including 13 million new infections.
3. There is no cure for HPV infection
Most HPV infections occur among teens, and once you are infected, there is no cure. There are treatments for some of the health problems that HPV can cause, such as genital warts and certain pre-cancers and cancers, but prevention is far better than treatment.
4. HPV vaccination helps keep children and young adults healthy
It can take 15-20 years after an HPV infection occurs for cancer to develop in people with normal immune systems and 5-10 years in those with weakened immune systems. The best way to avoid infection is to get vaccinated before the start of any sexual activity. Studies have also shown that the earlier you get vaccinated, the more protective it is.
HPV vaccine is recommended for both males and females.
5. HPV vaccines are safe and effective
HPV vaccines have been proven to be safe and effective at preventing HPV-related infections and cancers. Many people who get vaccinated against HPV have no side effects and among those who do, the most common side effects are usually mild, like a sore arm or redness at the injection site.
To help protect against HPV infection, CDC recommends HPV vaccination for:
- All preteens age 11 or 12 years (vaccination can start as early as age 9 years)
- Everyone up to age 26 years, if not vaccinated already
Adults age 27-45 years should talk with a healthcare professional about whether HPV vaccination is right for them and if they are likely to benefit from vaccination.
Learn more at: www.nfid.org/hpv
Resources for Healthcare Professionals
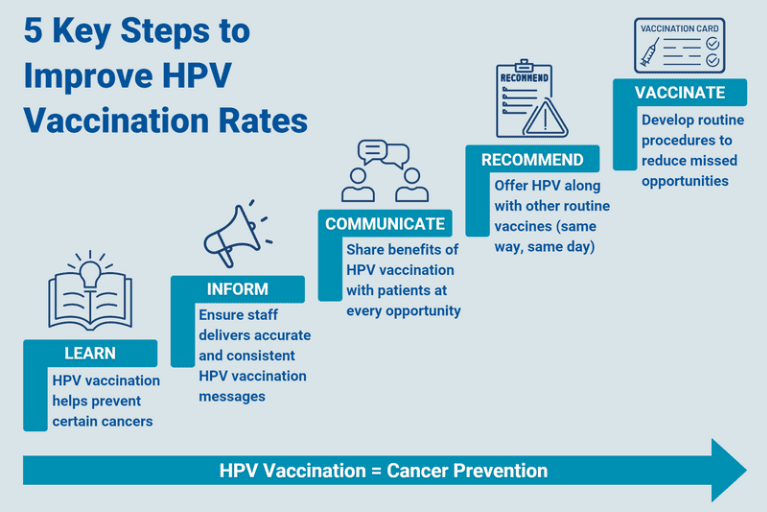
To increase HPV vaccination rates, research shows that healthcare professionals (HCPs) working with preteens, teens, and young adults should make a strong recommendation for HPV vaccination and clearly indicate that HPV vaccination is cancer prevention. The National Foundation for Infectious Diseases (NFID) has developed resources to help HCPs talk with their patients about the importance of HPV vaccination:
- Complimentary on-demand webinars on Cancer Prevention through HPV Vaccination, Reducing Sexually Transmitted Infections (STIs) through Effective Prevention and Treatment, and more at: www.nfid.org/webinars
- Downloadable infographic highlighting 5 steps HCPs can take to make HPV vaccination routine among patients:
To join the conversation and get the latest news on infectious diseases, follow NFID on Twitter using the hashtags #PreventHPV and #StopHPVCancer, like us on Facebook, follow us on Instagram, visit us on LinkedIn, listen and subscribe to the Infectious IDeas podcast, and subscribe to receive future NFID Updates.
Related Posts
The Key to Preventing Cervical Cancer
January is Cervical Cancer Health Month, an important time to raise awareness and empower individuals to protect themselves against this often preventable type of cancer

ID News Round-Up: Bird Flu, COVID-19, HPV, and Norovirus
Read recent news of interest from the world of infectious diseases including insights and explanations on bird flu, COVID-19, HPV, and norovirus …
2 Simple Steps to Prevent Cervical Cancer
Vaccination helps protect against cervical cancer and other cancers caused by HPV