 To highlight the importance of annual flu prevention, NFID is sponsoring a blog relay during 2016 National Influenza Vaccination Week (NIVW), featuring guest posts authored by NFID leaders each day of the week.
To highlight the importance of annual flu prevention, NFID is sponsoring a blog relay during 2016 National Influenza Vaccination Week (NIVW), featuring guest posts authored by NFID leaders each day of the week.
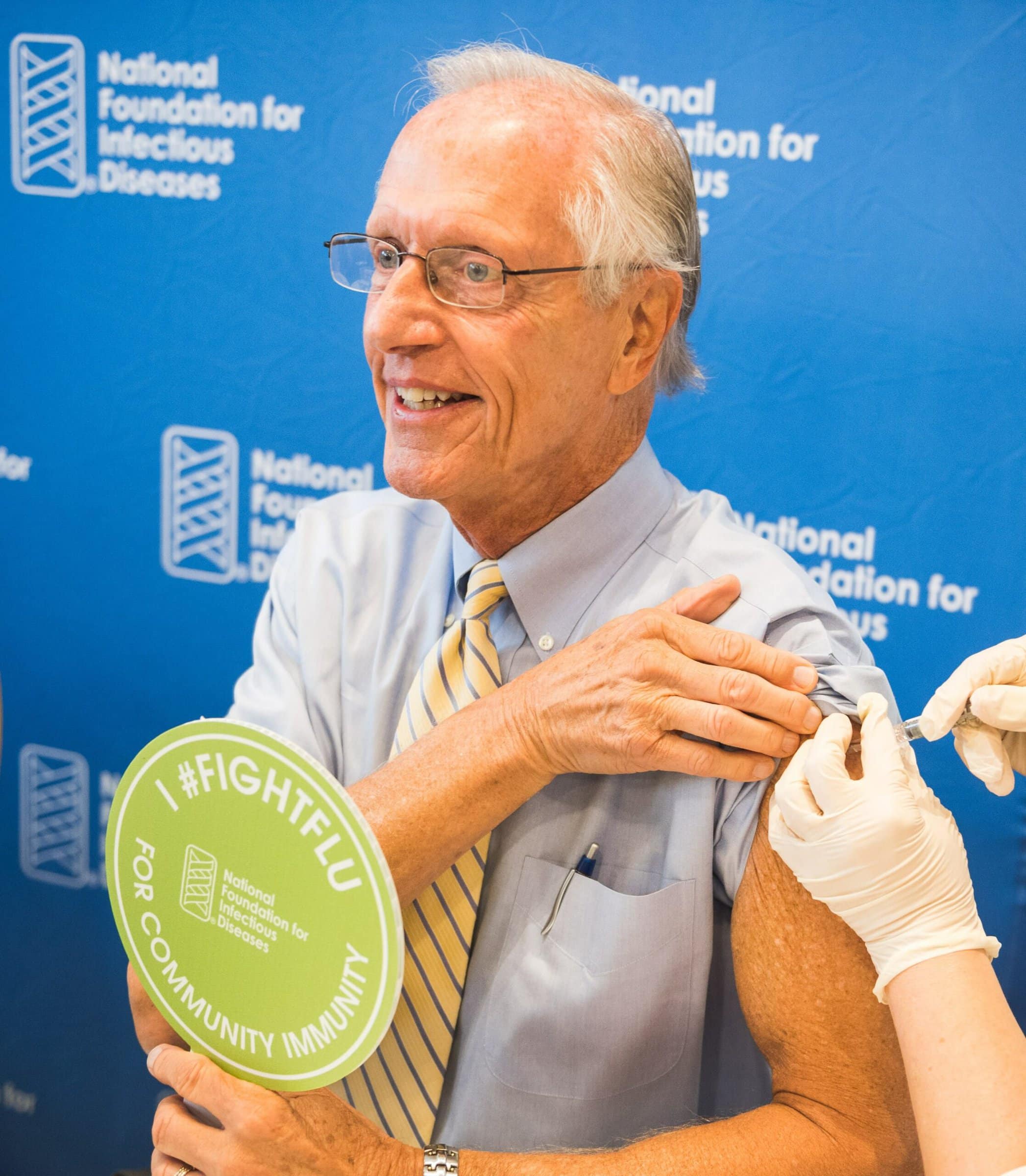
Special thanks to William Schaffner, MD, NFID Medical Director and Professor of Preventive Medicine and Infectious Diseases at Vanderbilt University School of Medicine, for this guest post highlighting changes in influenza immunization over the past 20 years.
The first recorded worldwide influenza epidemic happened in 1580, more than 430 years ago. The outlook for preventing influenza remained bleak for 350 years until the first influenza virus strain was isolated in a laboratory in 1933, and the work began to create an effective vaccine.
In the 80+ years since, we have advanced past vaccines that protect against just one influenza strain, to vaccines that protect against two, three, and even four strains. This is very important, as it is common for more than one influenza strain to circulate simultaneously in communities. We have also moved past the one-size-fits-all vaccine model, with tailored vaccines available for adults age 65 years and older, those with needle-phobia, and people with (very rare) severe egg allergies.
And it is not just the vaccines that have changed. When the National Foundation for Infectious Diseases (NFID) hosted its first annual influenza news conference to kick off the influenza vaccination season 20 years ago, the Centers for Disease Control and Prevention (CDC) recommended routine influenza vaccination only for adults age 65 years and older.
Today annual influenza vaccination is recommended for all individuals age six months and older…
Twenty years ago, approximately 40 million individuals in the US were included in the routine influenza vaccination category (and not all of them were vaccinated). During the 2015-2016 season, CDC estimates that about 144 million people in the US received an influenza vaccine.
We have progressed from past worries about whether there would be sufficient vaccines with supply available early enough in the season. The number of manufacturers supplying the US market and their overall production capacity has increased steadily, which has led to a remarkably stable influenza vaccine supply that typically becomes available in the US as early as August each year. We also have a large and growing choice of locations where individuals can get vaccinated. In addition to traditional doctors’ offices, public health clinics, and hospitals, influenza vaccination locations now include workplaces, community centers, schools, and pharmacies, among others. Many locations offer the public a very convenient option—some are even open 24 hours and few require an advance appointment.
The ultimate question, though, is whether this stable and growing influenza vaccine supply is getting into the arms of those who need it. Frankly, I’m a glass half full guy. Despite some annual variability, our progress in protecting more people from influenza by vaccination each year has been steady. Of course, some groups do better than others.
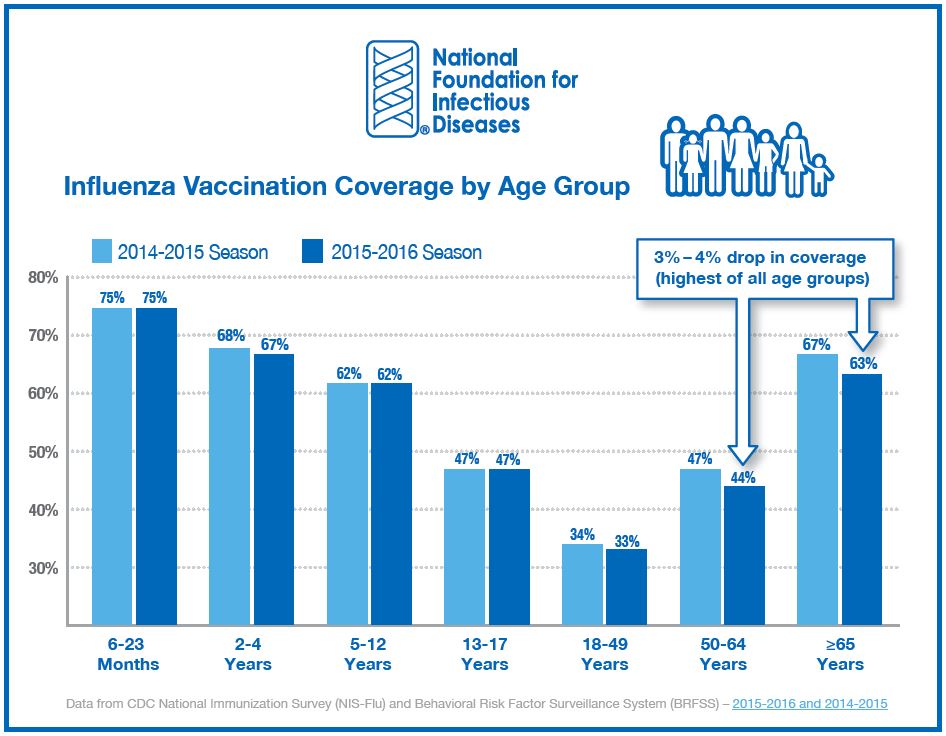
US vaccine coverage was basically flat last season compared to the previous season, but there were some losses in coverage for the 50-64 and 60+ age groups. We need to keep pushing past any complacency to keep vaccination rates moving upward.
Children younger than age five years and, despite last year’s slight drop, adults age 65 years and older, have the highest influenza vaccine coverage overall. But 25 percent or more remain unprotected in each of these age groups. We have made terrific progress, but as long as people are getting sick, being hospitalized, and dying from this preventable infection, we must strive to do better.
Although not called out specifically in the chart above, congratulations are certainly due to our nation’s healthcare professionals (HCPs) for Leading by Example each year: four in five got their influenza vaccine last season (79%) and nearly all physicians in the US were vaccinated last season (95.6%). That’s a glass close to overflowing! We have made significant advances in immunizing ourselves as HCPs, now we need to do for our patients what we do for ourselves. Working together, we can continue to help prevent even more cases of influenza each year.
Be sure to check NFID News each day during #NIVW to view guest blog posts, including the upcoming post by Lisa S. Ipp, MD about the impact of flu on teens and college students.
To join the conversation, follow NFID on Twitter (@nfidvaccines) using the hashtag #FightFlu and #NIVW, like us on Facebook, join the NFID Linkedin Group, and subscribe to NFID Updates.
Related Posts

News Round-Up: Infectious Disease Threats
According to NFID website poll, there are several worrisome infectious disease threats. Read recent news on topics of greatest concern, including avian influenza (bird flu), measles, and respiratory syncytial virus (RSV) …

Vaccines and Heart Health: A Vital Connection
Heart disease can increase the risk of serious or fatal complications from respiratory diseases including COVID-19, flu, and RSV

Harnessing the Power of Local Data
NFID dashboard aims to empower stakeholders with hyperlocal data to increase US adult respiratory vaccine uptake