Special thanks to NFID Board member Beth P. Bell, MD, MPH, former director, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention (CDC), for this guest blog post focused on the importance of appropriate antibiotic use during US Antibiotic Awareness Week (November 13-19, 2017).
Each year in the US, at least 2 million individuals get sick from antibiotic-resistant infections and more than 23,000 people die as a result of these infections. Antibiotics are life-saving medications that have played a key role in many successes of modern medicine. However, our toolkit for fighting antibiotic-resistant infections, especially those caused by “superbugs” resistant to most, or all, antibiotics, is perilously close to empty. The rise of antibiotic resistance is currently one of the world’s most serious health threats.
Using antibiotics increases the resistance to them because microbes constantly change and evolve to escape being killed by the antibiotics. Antibiotic resistance can spread in hospitals, long-term care facilities, and other healthcare settings, as well as in the community from patients who harbor resistant bacteria after having been treated with antibiotics. Infections can also be spread to humans from animals with antibiotic-resistant bacteria. Infections may occur because of contact with uncooked or improperly cooked meat from these animals or from food crops that have come into contact with contaminated water or runoff.
Everyone has a role to play in preventing antibiotic resistance. Avoiding infections in the first place reduces the need for antibiotics so simple preventive measures like staying up-to-date on all recommended vaccinations, cooking meat thoroughly, practicing good hygiene including proper handwashing, and taking antibiotics only when necessary and as prescribed, are smart steps all individuals can and should take.
New drugs and diagnostics are also an important part of the solution. Microbes are constantly developing new ways to avoid the effects of antibiotics, so antibiotic resistance cannot be stopped, only slowed. We will always need new antibiotics in the development pipeline and new diagnostics to track resistance and guide antibiotic prescribing.
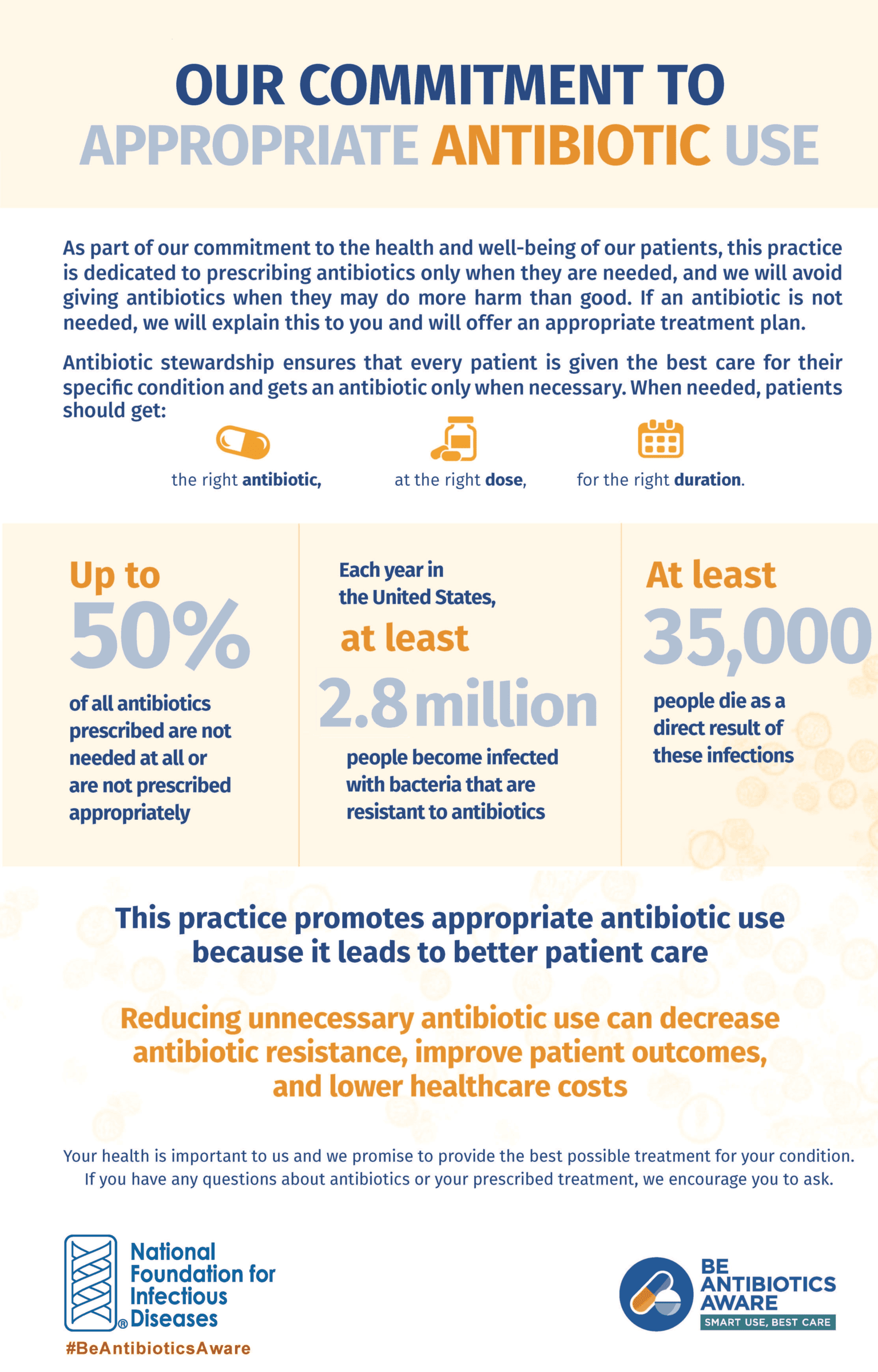 Perhaps the most important intervention in slowing the spread of antibiotic resistance is to change the way antibiotics are used. CDC estimates that up to 50% of all antibiotics used in healthcare and much of the antibiotic use in animals are unnecessary. We need to reduce the amount of antibiotics used in animals and support healthcare professionals (HCPs) in making the appropriate determination when antibiotics are needed. NFID has developed an Antibiotic Stewardship Pledge that HCPs can use to visibly share their commitment to appropriate antibiotic prescribing with patients and colleagues.
Perhaps the most important intervention in slowing the spread of antibiotic resistance is to change the way antibiotics are used. CDC estimates that up to 50% of all antibiotics used in healthcare and much of the antibiotic use in animals are unnecessary. We need to reduce the amount of antibiotics used in animals and support healthcare professionals (HCPs) in making the appropriate determination when antibiotics are needed. NFID has developed an Antibiotic Stewardship Pledge that HCPs can use to visibly share their commitment to appropriate antibiotic prescribing with patients and colleagues.
Only by stewarding our existing antibiotic supply and encouraging HCPs to use the right antibiotics, at the right dose, for the right duration, and only when needed, will we be able to prevent further antibiotic resistance. CDC has developed guidelines for stewardship programs that have been endorsed by many professional organizations. These guidelines need to be implemented across all aspects of healthcare, including veterinary care.
It is not too late to slow the spread of resistant bacteria. Prevention is key! Working together, we must identify and stop outbreaks faster, track the spread of disease more quickly, and improve the way antibiotics are used in healthcare and agriculture to preserve the effectiveness of these precious medicines.
To learn more, view the NFID webinar, Be Antibiotics Aware: Smart Use, Best Care, and access other valuable resources at www.nfid.org/amr.
To join the conversation, follow NFID on Twitter using the hashtags #AntibioticSmart and #BeAntibioticsAware, like NFID on Facebook, follow NFID on Instagram, join the NFID Linkedin Group, and subscribe to NFID Updates.
Related Posts

Protecting Children as They Head Back to School
As school gets underway, experts from the National Foundation for Infectious Diseases (NFID) offer insights on childhood immunization
Lifelong Conversations about Sexual Health
Teen Health Week is April 4-10, 2022, and STD Awareness Week is April 10-16, 2022, both of which provide an opportunity for healthcare professionals to begin lifelong conversations with patients about sexual health and the importance of staying up to date on all recommended vaccines …
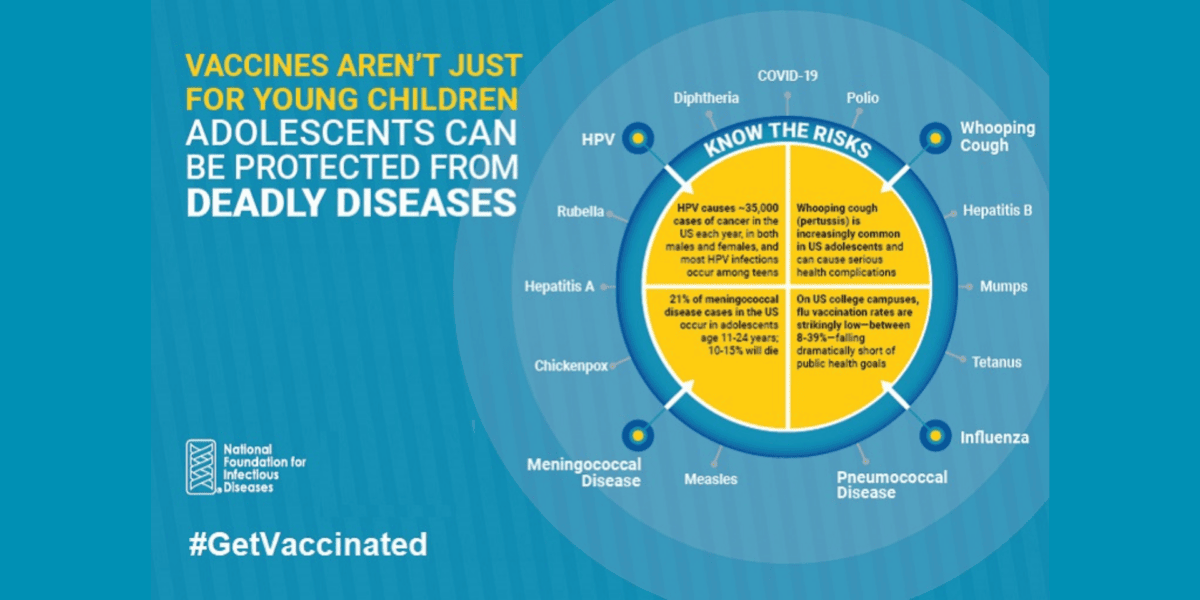
Vaccines Are Not Just for Young Children
CDC recommends vaccinations from birth to adulthood to provide a lifetime of protection. Yet many adolescents are not vaccinated as recommended, leaving them unnecessarily vulnerable. International Adolescent Health Week (March 20-26, 2022) is a perfect time to make sure that pre-teens and teens are up to date on all recommended vaccines …
